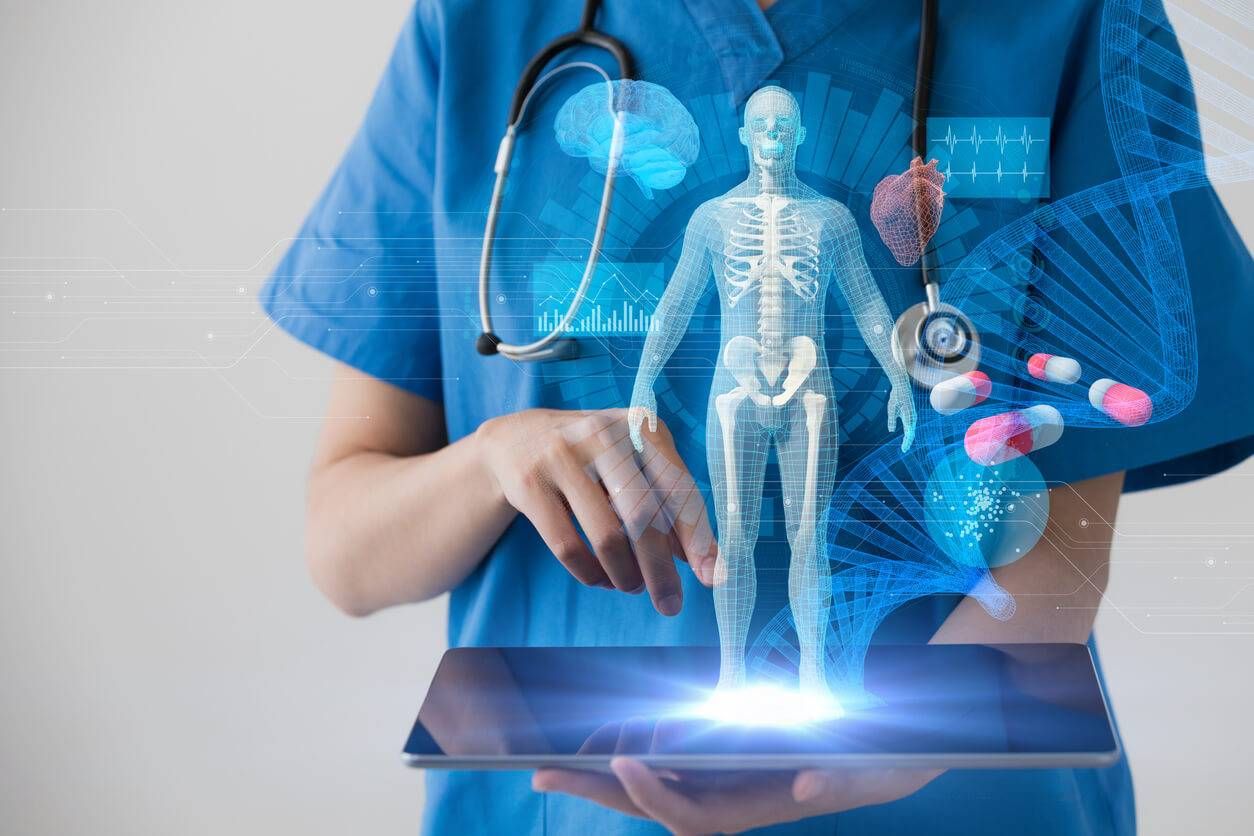
The landscape of modern medicine is undergoing its most significant transformation since the discovery of penicillin. This revolution isn’t being driven by a new wonder drug, but by a powerful and pervasive force: Artificial Intelligence (AI). Far from the realm of science fiction, AI has become a critical, integrated component in hospitals, research labs, and clinics worldwide. It is a technological undercurrent that is fundamentally reshaping how we diagnose diseases, develop treatments, manage patient care, and unlock the very secrets of human biology.
For decades, healthcare has been a field rich in data but often poor in its ability to connect the dots in a timely and efficient manner. Patient records, medical images, genomic sequences, and clinical trial results create a deluge of information that is impossible for the human mind to process comprehensively. AI, with its capacity for machine learning and deep learning, is uniquely equipped to navigate this complexity. It can identify patterns, predict outcomes, and automate tasks with a level of speed and accuracy that was previously unimaginable.
This profound integration of AI is not merely an incremental improvement; it’s a paradigm shift. It’s about augmenting the capabilities of our brilliant doctors and researchers, freeing them from routine, data-intensive tasks to focus on what they do best: providing compassionate, human-centric care. From predicting septic shock hours before symptoms appear to designing novel drugs at a fraction of the traditional cost, AI is ushering in a new era of proactive, personalized, and precision medicine. This article explores the multifaceted role of AI in healthcare, delving into its groundbreaking applications, the challenges it presents, and the extraordinary future it promises.
A. AI in Diagnostics: Seeing the Unseen
Perhaps the most impactful application of AI in healthcare today is in the field of diagnostics, particularly medical imaging. Radiologists, pathologists, and other specialists are tasked with identifying subtle abnormalities in a sea of visual data—a process that is both time-consuming and subject to human error. AI, specifically deep learning algorithms, is proving to be an invaluable partner in this critical task.
- Elevating Medical Imaging Analysis: AI models can be trained on millions of medical images (X-rays, CT scans, MRIs) to recognize signs of disease with superhuman accuracy. For instance, AI algorithms are now capable of detecting cancerous tumors in mammograms and lung nodules on CT scans at a far earlier stage than the human eye. This doesn’t replace the radiologist; it acts as a powerful screening tool, flagging suspicious areas so that experts can focus their attention where it’s needed most, leading to earlier diagnoses and significantly improved patient outcomes.
- The Rise of Predictive Diagnostics: Beyond just identifying existing diseases, machine learning models are being used to predict the likelihood of future health events. By analyzing a patient’s electronic health record (EHR), genetic information, and lifestyle factors, AI can calculate their risk for developing conditions like heart disease, diabetes, or even certain types of cancer. This allows clinicians to intervene proactively with preventative care strategies tailored to the individual.
- Democratizing Expertise: In many parts of the world, access to specialist diagnosticians is limited. AI-powered diagnostic tools can help bridge this gap. A primary care physician in a rural clinic could use an AI-powered smartphone app to screen for diabetic retinopathy, a leading cause of blindness, enabling early referral and treatment without the immediate need for an ophthalmologist.
B. Transforming Drug Discovery and Development
The journey of bringing a new drug to market is notoriously long, expensive, and fraught with failure. It can take over a decade and billions of dollars, with a high percentage of candidates failing in late-stage clinical trials. AI is drastically changing this equation by streamlining and accelerating nearly every phase of the process.
- Identifying Novel Drug Targets: The first step in creating a new drug is understanding the biological origin of a disease. AI can analyze vast datasets of genetic and proteomic information to identify novel protein targets that are likely to respond to therapeutic intervention. This initial step, which could traditionally take years of lab research, can now be accomplished in a fraction of the time.
- Designing Better Molecules: Once a target is identified, AI algorithms can predict which molecular compounds are most likely to be effective and have the fewest side effects. These systems can design and test millions of potential drug molecules in silico (on a computer), ensuring that only the most promising candidates move on to expensive and time-consuming physical lab testing.
- Optimizing Clinical Trials: AI is also revolutionizing how clinical trials are run. Machine learning can help researchers identify the ideal patient cohorts for a trial, predict which participants might drop out, and monitor for adverse events in real-time. This leads to faster, more efficient, and more successful trials, getting life-saving treatments to patients sooner.
C. The Dawn of Personalized Medicine
For too long, medicine has operated on a one-size-fits-all model. Treatment plans were based on the “average” patient, which meant they were not perfectly optimized for anyone. AI is the engine driving the shift towards personalized medicine, where treatments are tailored to an individual’s unique genetic makeup, lifestyle, and environment.
- Customized Treatment Protocols: In oncology, AI is being used to analyze a patient’s specific tumor genomics to determine the most effective combination of chemotherapy drugs or targeted therapies. This moves beyond treating “lung cancer” to treating a specific individual’s unique form of lung cancer, drastically increasing the chances of a positive response.
- Dynamic Treatment Adjustment: AI-powered systems can continuously monitor a patient’s response to treatment through wearable devices and other data sources. For a diabetic patient, an AI system could analyze real-time glucose data and recommend adjustments to their insulin dosage or diet on the fly. This creates a dynamic feedback loop that optimizes care continuously.
D. Streamlining Healthcare Operations and Administration

The burden of administrative tasks is a major contributor to clinician burnout and healthcare costs. AI is a powerful tool for automating these workflows, freeing up medical professionals to spend more time with their patients.
- Intelligent Workflow Automation: AI can handle tasks like medical coding, billing, and managing insurance claims, reducing errors and saving countless hours of manual work. Voice recognition AI can also transcribe doctor-patient conversations directly into the electronic health record, eliminating the need for tedious manual note-taking.
- Optimizing Hospital Operations: Hospitals are complex systems. AI algorithms can optimize patient scheduling to reduce wait times, predict patient admission rates to manage bed capacity, and even manage supply chain logistics to prevent shortages of critical medical supplies.
E. AI and Robotics in Surgery
The operating room is another area where AI is making a significant impact. While the concept of a “robot surgeon” is still futuristic, AI-assisted robotics are enhancing the precision, skill, and safety of human surgeons today.
- Enhanced Surgical Precision: Robotic systems controlled by surgeons provide a magnified, 3D view of the surgical site and enable more precise movements than the human hand is capable of. AI adds a layer of intelligence, providing real-time data overlays, highlighting critical structures like nerves or blood vessels, and even helping to steady the surgeon’s instruments to minimize tremors.
- Data-Driven Surgical Insights: AI platforms can analyze thousands of hours of surgical video to identify best practices and techniques correlated with the best patient outcomes. This data can be used to train new surgeons and provide established surgeons with insights to help them refine their skills.
Challenges and Ethical Considerations
The integration of AI into healthcare is not without its challenges. Issues of data privacy, algorithmic bias, and accountability are paramount. AI models are only as good as the data they are trained on, and if that data reflects existing biases in healthcare, the AI can perpetuate or even amplify them. Furthermore, determining liability when an AI-assisted diagnosis is incorrect is a complex legal and ethical question that society is still grappling with. Transparency in how these algorithms work and ensuring robust regulatory oversight are critical steps to building trust and ensuring AI is deployed safely and equitably.
The future of healthcare is a collaborative one—a partnership between human expertise and artificial intelligence. AI will not replace doctors, but doctors who use AI will undoubtedly replace those who do not. By embracing this powerful technology, we can build a future where healthcare is more predictive, more personalized, and more accessible for everyone on the planet.